Obesity Care Model Collaborative (OCMC)

While there are many different treatment options for patients diagnosed with obesity, a reliable and universally accepted care model does not exist. AMGA Foundation aimed to change this through its Obesity Care Model Collaborative (OCMC), a three-year initiative that provided a framework for expanded work on the disease.
The OCMC brought medical groups and health systems from across the country together to share strategies and best practices for treating obesity. Participating organizations also submitted obesity care data to AMGA, which synthesized, analyzed and reported on any data trends discovered.
This data, combined with the anecdotal evidence participants gathered from their peers has been used to create a reliable framework for successfully treating obesity.
OCMC was also supported by an Advisory Committee of physicians and quality improvement experts to help guide the development of the collaborative.
The following are several interventions OCMC participants have implemented as a result of the program
-
Obesity Clinic: A new clinic was created as a strategy to address obesity in the patient population.
-
Obesity Support Group: A physician-led community support program was created for patients suffering from obesity.
-
Shared Medical Appointments: Group appointments for obesity and diabetes, obesity and comorbidities, and obesity and chronic pain were expanded.
-
Metabolic Care Program: A program focusing on culinary medicine was launched.
-
“Weight for You” Program: This three-month program focused on obesity and primary care.
-
Community Garden/Food Pharmacy: A garden and healthy food bank was created to engage community members while providing healthy food for patients and the larger community.
-
Community Partnership: A partnership was formed between a member and a third-party organization to establish a social media-based cooking class.
-
Community Resources: Hospitals and clinics established centers to identify patient resources within the community and provide patients with information about them.
-
Reducing Disparities: Three members began assessing of their organization’s obesity care framework as it relates to equity.
-
Nurse Navigator: A new position was created to assist providers caring for patients with obesity and to connect patients with available resources.
-
Best Practice Alerts: A system of alerts for documenting BMI was implemented into an EMR.
-
Clinic Environment: Several groups made environmental changes to better accommodate patients with obesity (i.e., larger blood pressure cuffs, larger gowns, wider chairs in waiting area, etc.). One group designated an exam room in each practice specifically to patients with obesity.
-
Patient Champions: Patient champions were selected to directly represent the interests of stakeholders during the development of obesity care programs.
“The obesity data AMGA collected and analyzed throughout this program has been extremely valuable. This data can’t be found anywhere else, though; it’s unique to this program and the providers in it.”
– Timothy Garvey, M.D., Professor and Chair, Department of Nutrition Sciences, University of Alabama Birmingham
“Knowledge and best practices are meant to be shared, and these meetings allow us to do just that. This collaborative has exposed us to new ideas and strategies, many of which we may never have thought of on our own.”
– Marianne Sumego, M.D., Physician, Community Internal Medicine, Cleveland Clinic
“This program empowers better practice and influences the delivery of higher quality care. AMGA’s staff does a remarkable job, and I’m very thankful for the opportunity to be a participant!”
– 2018-2019 OCMC Participant
The OCMC generated a number of resources meant to serve as guidelines to help medical groups and health systems improve their own obesity care delivery efforts.
OCMC Playbook
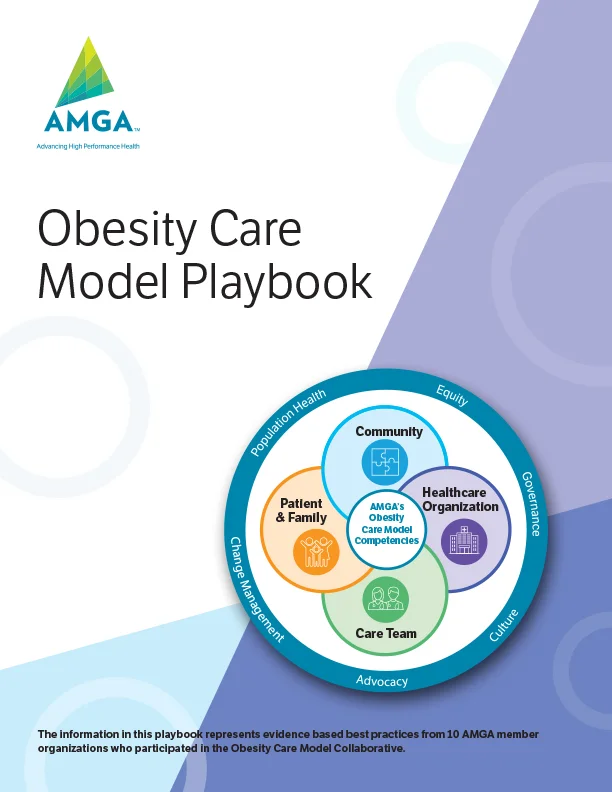
The OCMC Playbook provides users with knowledge and insights on population health-based approaches and strategies to treating adult patients with obesity in primary care.
The information in this playbook represents evidence-based best practices from AMGA member organizations who participated in the Obesity Care Model Collaborative.
White Paper | Cultivating a Comprehensive Obesity Program in Primary Care
This white paper provides a comprehensive overview of the OCMC, including information on how the collaborative came to be, its purpose, structure, outcomes, and key findings. Download the OCMC white paper
-
Advocate Aurora Health
FTE: 3,285 -
Cleveland Clinic
FTE: 3,038 -
Confluence Health
FTE: 292 -
Guthrie Clinic
FTE: 298 -
HealthCare Partners
FTE: 500
-
The Iowa Clinic
FTE: 115 -
Mercy Clinic East Communities
FTE: 549 -
Novant Health
FTE: 1,380 -
Tulane University Medical Group
FTE: 326 -
Utica Park Clinic
FTE: 262
The OCMC generated a number of articles published in both peer-reviewed academic journals, and editorial publications.
Building Successful Models in Primary Care to Improve the Management of Adult Patients with Obesity (Research)
Casanova, D., Kushner, R. F., Ciemins, E. L., Smolarz, B. G., Chambers, E., Leaver-Schmidt, E., Kennedy, J. W., & Garvey, W. T. (2021). Population Health Management, Ahead of Print, 30 March 2021
Your Say
February 24, 2021
By Elizabeth Ciemins, Ph.D., M.P.H., M.A.
Modern Healthcare,
January 01, 2021
By Maria Castellucci
Istfan, N. W., & Apovian, C. M. (2020). Obesity, 28(12), 24 November 2020
Measuring What Matters: Beyond Quality Performance Measures in Caring for Adults with Obesity (Research)Ciemins, E.L., Joshi, V., Horn, D., Nadglowski, J., Ramasamy, A., Cuddeback, J., (2020). Population Health Management, Ahead of Print, 11 November 2020
Diagnosing Obesity as a First Step to Weight Loss an Observational Study (Research)
Ciemins, E.L., Joshi, J., Cuddeback, J.K., Kushner, R.F., Horn, D.B., Garvey, W.T., (2020). Obesity, Early View, 07 October 2020
(Research)
Advisory Committee
The Obesity Care Model Collaborative (OCMC) is a program development collaborative with an objective to pilot, define, and evaluate a framework and necessary components to address obesity in patients served by multispecialty medical groups and integrated health systems. Two committees (program development and measurement) of expert advisors are drafting the framework and measures, and developed the inclusion criteria for selection of AMGA member organizations to participate in a population-based approach to obesity management for patients treated in primary care. Advisors have been selected based on their expertise in key competencies and experience in managing patients with obesity.
Ten AMGA member groups were selected based on their ability to contribute to the further development of the framework, test measures, and their commitment to implement an obesity program that includes a minimum range of services, either within the group or through referral partnership. Each organization have selected a representative to serve on the advisory committee. Participating organizations will meet in-person four times, plus via a series of webinars, to share insights and challenges and to refine the framework and measures based on the data and their experiences. Facilitation and support of the implementation is being provided by the AMGA Foundation including administrative support, telephonic and onsite support, online tools and resources, monthly educational webinars and data/analytic support.
OCMC is presented by AMGA Foundation in collaboration with Novo Nordisk, Inc. The collaborative is also supported by an Advisory Committee of physicians and quality improvement experts to help guide the development of the collaborative:
Doris M. Boutain, Ph.D., R.N., John and Marguerite Walker Corbally Professor in Public Service, University of Washington School of Nursing
Paula Burich, R.N., B.S.N., Director, Sharp Rees-Stealy Center for Health Management
Barto Burguera, M.D. Ph.D., Professor of Medicine, Director of Obesity Programs, Cleveland Clinic
Timothy Garvey, M.D., Professor of Medicine and Chair, Department of Nutrition Sciences, University of Alabama at Birmingham, American Association of Clinical Endocrinologist (AACE)
Gina Gordon, R.N., RD, L.D.N., Manager, Bariatric Program, Novant Health
Timothy Harlan, M.D., FACP, Executive Director, Goldring Center for Culinary Medicine, Tulane University Medical Group
Barbara Hodne, D.O., Associate Quality Director, The Iowa Clinic
Deborah Horn, D.O., M.P.H., Medical Director, UT Center of Obesity Medicine and Metabolic Performance, Obesity Medicine Association
Robert Kushner, M.D., Past President, The Obesity Society
Natasha Malesevich, M.H.A., Senior Project Manager, Strategic Operations - Transformation Team, Aurora Health Care
Kara Mayes, M.D., Family Medicine Physician, Mercy Clinic
Kathleen Morton, M.D., Internist, Coastal Medical, East Providence
Kathy Mostafaie, M.D., Medical Director, HealthCare Partners
Joe Nadglowski, President/CEO, Obesity Action Coalition
Michelle O’Meara, D.O., Bariatric Physician, Utica Park Clinic
Marianne Sumego, M.D.
Staff Physician, Internal Medicine/Pediatrics
Director, Shared Medical Appointments, Cleveland Clinic
Clinical Assistant Professor of Medicine CCLCM of CWRU
Andrew Toth, M.D., Family Medicine Physician, Confluence Health
Verlyn Warrington, M.D., Medical Director, Bariatric Medicine, The Guthrie Clinic