Improving Care Transitions for Patients with Venous Thromboembolism (VTE)

Issue
Venous thromboembolism (VTE) manifests as symptomatic or asymptomatic deep vein thrombosis (DVT) that can lead to a potentially fatal pulmonary embolism (PE). VTE is among the most common causes of preventable hospital death and readmissions are often longer and more costly than initial hospitalization. Most clots that occur in the outpatient setting can be linked to a recent hospitalization or surgery.
Project Objective
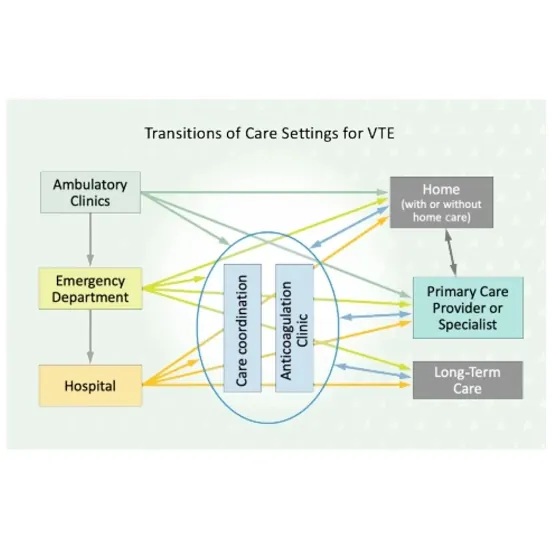
Together with a team of national experts, AMGA and 6 AMGA members conducted a quality improvement and implementation science study over 12 months to improve the quality of care transitions for patients with VTE between hospital, emergency department (ED), and ambulatory settings.
Understanding VTE as a serious population health issue
"What we lack are ongoing VTE protocols will help us incoporate action plants and continuity of care in our patient population with VTE... [and] will work well in our efforts to improve the health of our patients."
Positively impacting care by reducing costs and improving VTE care management
"...to further analyze and enhance our current program... as we strive to learn more about our currrent impact on quality, cost, and utilization, ...innovative and effective approaches to VTE transitions would be a substantial learning outcome."
Results
Participating healthcare organizations reduced hospitalizations and ED visits within 45 days of a VTE diagnosis by an average relative reduction of 18.7% (p=0.033) across all settings. Additionally, there was an overall average relative improvement of 33.3% (p=<0.0001) in follow-up within 7 days of a VTE diagnosis where follow-up included an ambulatory care visit, phone call, video visit, or electronic communication.
Interventions associated with improving 7-day follow-up after a VTE episode, reducing VTE-related 45-day readmissions, or both, included:
-
Improving communication across care teams;
-
Improving safe prescribing and management of anticoagulants;
-
Implementing standardized protocols and centralized care processes; and
-
Expanding the scope of the anticoagulation clinics to include patients on direct oral anticoagulants (DOACs).
Interventions
The following case studies describe the care gaps addressed by five AMGA members, including interventions implemented, available resources, and outcomes achieved within health systems.
North Mississippi Health Services,Tupelo, MS
Comprehensive care during care transitions (Bridge Award Winner)
Interventions: VTE patient registry, patient and prescriber education, primary care engagement
Alleghany Health Network (formerly Excela Health), Pittsburgh, PA
Improving communication and coordination between the hospital and primary care
Interventions: Hospital-based coordinator, care coordination software, prescribing error alerts, patient phone calls
Henry Ford Health, Detroit, MI
Creating safer care transitions from the ED to home
Interventions: Follow up for patients outside of system, warm handoffs to external primary care providers
Independence Health System (formerly Excela Health), Greensburg, PA
Providing DOACs in primary care settings
Interventions: Follow up phone calls, DOAC starter packs in ambulatory setting
Beth Israel Lahey Health, Burlington, MA
Improving patient education for VTE
Interventions: Meds to beds program, auto referrals to anticoagulation clinic